Kidney Cancer Journal 55
2005 2006 2007 2008 2009 2010
There are hopeful signs, however, that new studies will
more definitively address all of these issues. Two prospective
randomized trials, the Clinical Trial to Assess the Importance
of Nephrectomy (CARMENA)5 and the European
Organisation for Research and Treatment of Cancer’s
Immediate Surgery or Surgery After Sunitinib Malate
in Treating Patients with Metastatic Kidney Cancer (SURTIME)
6 were designed to examine these issues. Still, the
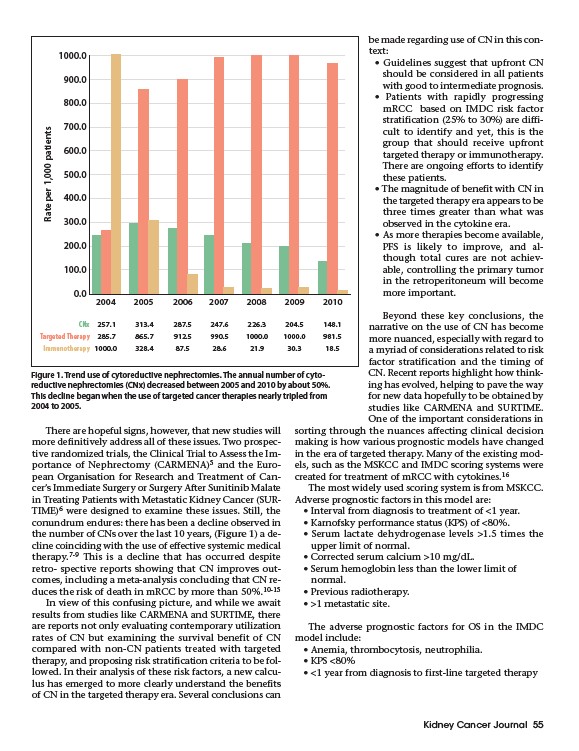
conundrum endures: there has been a decline observed in
the number of CNs over the last 10 years, (Figure 1) a decline
coinciding with the use of effective systemic medical
therapy.7-9 This is a decline that has occurred despite
retro- spective reports showing that CN improves outcomes,
including a meta-analysis concluding that CN reduces
the risk of death in mRCC by more than 50%.10-15
In view of this confusing picture, and while we await
results from studies like CARMENA and SURTIME, there
are reports not only evaluating contemporary utilization
rates of CN but examining the survival benefit of CN
compared with non-CN patients treated with targeted
therapy, and proposing risk stratification criteria to be followed.
In their analysis of these risk factors, a new calculus
has emerged to more clearly understand the benefits
of CN in the targeted therapy era. Several conclusions can
be made regarding use of CN in this context:
• Guidelines suggest that upfront CN
should be considered in all patients
with good to intermediate prognosis.
• Patients with rapidly progressing
mRCC based on IMDC risk factor
stratification (25% to 30%) are difficult
to identify and yet, this is the
group that should receive upfront
targeted therapy or immunotherapy.
There are ongoing efforts to identify
these patients.
• The magnitude of benefit with CN in
the targeted therapy era appears to be
three times greater than what was
observed in the cytokine era.
• As more therapies become available,
PFS is likely to improve, and although
total cures are not achievable,
controlling the primary tumor
in the retroperitoneum will become
more important.
Beyond these key conclusions, the
narrative on the use of CN has become
more nuanced, especially with regard to
a myriad of considerations related to risk
factor stratification and the timing of
CN. Recent reports highlight how thinking
has evolved, helping to pave the way
for new data hopefully to be obtained by
studies like CARMENA and SURTIME.
One of the important considerations in
sorting through the nuances affecting clinical decision
making is how various prognostic models have changed
in the era of targeted therapy. Many of the existing models,
such as the MSKCC and IMDC scoring systems were
created for treatment of mRCC with cytokines.16
The most widely used scoring system is from MSKCC.
Adverse prognostic factors in this model are:
• Interval from diagnosis to treatment of <1 year.
• Karnofsky performance status (KPS) of <80%.
• Serum lactate dehydrogenase levels >1.5 times the
upper limit of normal.
• Corrected serum calcium >10 mg/dL.
• Serum hemoglobin less than the lower limit of
normal.
• Previous radiotherapy.
• >1 metastatic site.
The adverse prognostic factors for OS in the IMDC
model include:
• Anemia, thrombocytosis, neutrophilia.
• KPS <80%
• <1 year from diagnosis to first-line targeted therapy
1000.0
900.0
800.0
700.0
600.0
500.0
400.0
300.0
200.0
100.0
0.0
Rate per 1,000 patients
2004
257.1 313.4 287.5 247.6 226.3 204.5 148.1
285.7 865.7 912.5 990.5 1000.0 1000.0 981.5
1000.0 328.4 87.5 28.6 21.9 30.3 18.5
CNx
Targeted Therapy
Immunotherapy
Figure 1. Trend use of cytoreductive nephrectomies. The annual number of cyto-
reductive nephrectomies (CNx) decreased between 2005 and 2010 by about 50%.
This decline began when the use of targeted cancer therapies nearly tripled from
2004 to 2005.